View and pay your medical bills online, get online price estimates for procedures and services, apply for financial aid, see billing explanations and more. The UC Student Health Insurance Plan (UC SHIP) UC SHIP offers a range of benefits, including coverage for specialty office visits, prescriptions, diagnostic services, surgery, hospitalization and out-of-area care while traveling, to name a few. The UC SHIP package also includes strong dental and vision benefits and covers most SHC fees. A copay, short for copayment, is a fixed amount a healthcare beneficiary pays for covered medical services. The remaining balance is covered by the person's insurance company. A copayment is a set fee the member pays to providers at the time services are provided. Copays are applied to emergency room visits, hospital admissions, office visits, etc. The cost is usually minimal. The patient should be aware of the copayment amounts prior to services being rendered. Talk to a doctor 24/7 by phone or video with Virtual Visits, a telehealth service offering treatment and prescriptions, as needed, for common health conditions.
We’ve answered some of the most commonly asked questions about health insurance to help break down what things are, how they work and what you can expect from your care.
- Networks & ID Cards
- Updating Your Information
- Changing or Shopping for Plans
- Claims, Coverage & Costs
- Pharmacies & Prescriptions
A network is a group of doctors we work with to provide care to our members. Providers in our network agree to offer our members a discount. Providers who aren’t in our network don’t offer that discount, so their rates are higher.
To find your network, look at the front of your Member ID card. It’s most likely on the bottom left corner.
How do I find out if my provider’s in network or find one who is?You can search for providers by network in the Find Care tool. Either search the provider’s name and check which networks they’re in, or search for providers near you and filter your results by your network. If you log in at bcbst.com, your search results will automatically list providers in your network.
What happens when I see a provider who’s not in my network?That depends on your plan benefits. For most plans, if you see a provider who is not in your network, subject to your out-of-network deductible and coinsurance. In that case, we typically pay the amount that we’d pay a provider who is in your network, subject to your out-of-network deductible and coinsurance. You’ll pay whatever is left on your bill. Please keep in mind that some plans, like those you may have purchased through Healthcare.gov or signed up for through TennCare, don’t pay for providers who aren’t in your network.
What if I need care when I’m traveling?This depends on what kind of plan you have.
Many employer plans include the Blue Cross Blue Shield Global Core® travel program that lets you see providers in other BlueCross networks while you’re traveling. If you see a small suitcase icon on your member ID card, then you have Global Core. If you’re planning a trip and have specific questions, the best thing to do is call Global Core directly at 1-800-810-25831-800-810-2583. They’re ready to help you out.
If you have an individual or family plan, or one through your employer, you can log in to bcbst.com and enter your location into the Find Care tool.
Medicare members should contact us, and we’ll help you decide how to get care.
Medicaid or Medicare with Medicaid members can only get coverage for providers out of the state of Tennessee if it’s a true emergency.
How do I get a new Member ID card?You can order a new Member ID card by logging in to bcbst.com or by calling or chatting with us.
You can also download a digital version or print your own copy of your card from the same page or you can see it in the myBlueTN℠ mobile app, which you can download here.
How do I change incorrect info on my Member ID card?Click here to contact us, and we’ll walk you through getting your card updated.
How do I update personal info like my address, last name or payment information?Click here to contact us, and we’ll get your account updated.
How do I add or remove a dependent?Click here to contact us, and we’ll get your account updated.
If you want to see a different doctor than the one you were assigned, you can contact us for help, or you can do it yourself here.
How/when can I enroll in or switch an Individual or Family plan?You’ll need to enroll during the Open Enrollment Period from Nov. 1 – Dec. 15 of each year. If you’ve had a major life change (like getting married, losing your coverage, moving out of state, etc.), you could shop now with a special enrollment window for a limited time. There’s more about that here.
How/when can I enroll in or switch my Employer's plan?Your employer likely has an enrollment window each year for you to sign up, unless you’re a new employee. Talk with your HR team about how to get enrolled.
How/when can I enroll in or switch a Medicare plan?You’ll need to shop during the Annual Enrollment Period, from Oct. 15 – Dec. 7 each year to switch plans. If you’re just turning 65 or retiring, you have a window of three months before and three months after your birthday to sign up for Medicare. Some big life events – like getting married or moving – might allow you to enroll in a plan outside this window. If you have one coming up, contact us or your broker.
How/when can I enroll in or switch a Medicare with Medicaid (BlueCare Plus℠) plan?If you qualify for both Medicare and Medicaid, you may sign up for a BlueCare Plus℠ plan throughout the year. Contact us or your broker to get help.
We want you to feel confident in making your Medicare decisions. Here’s a link to get you caught up on the basics or you can give our sales team a call at 1-800-292-51461-800-292-5146.
You can also visit our Medicare website for more information.
You can check your coverage by logging in here. This will give you all the details on who and what your plan covers. Or click here to contact us, and we'll look it up and help you with the next steps if we don't cover a service you need.
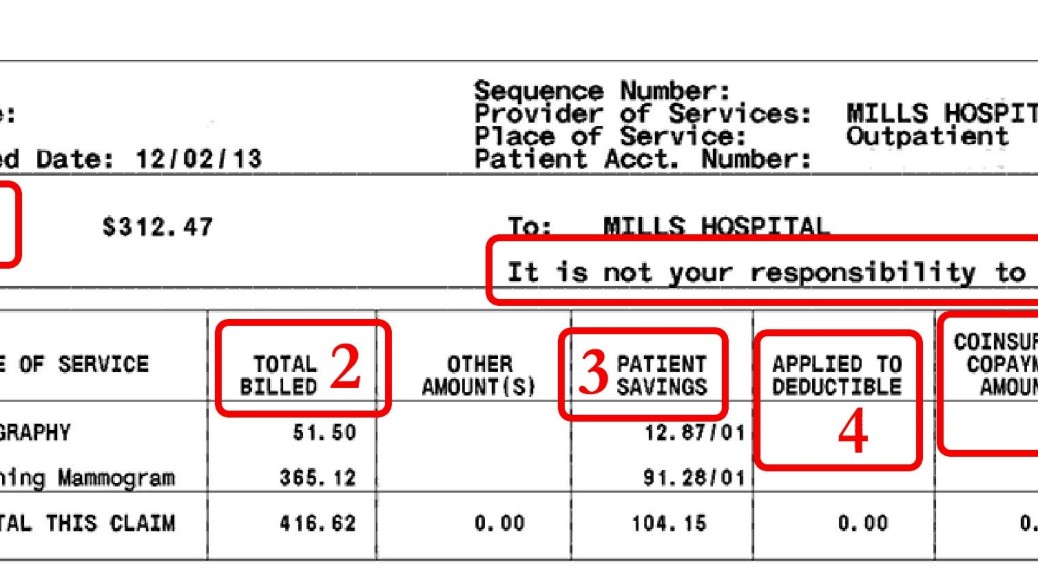
I’m confused about or disagree with a claims statement or bill. What do I do?Click here to contact us, and we’ll walk you through it. You can also watch this quick video that might help introduce you to the Claim Summary.
How do I pay my providers online?We offer free online bill pay for members with individual and employer plans. Log in to your account to view your claims. Pick the one you want to pay, then click the Pay Provider button. It will take you to InstaMed’s site, where you can make a full or partial payment.
What does “premium/copay/deductible/coinsurance” mean?Here’s a quick definition for the most common terms you’ll see in insurance:
Premium: The monthly payment for your insurance policy.
Copayment (Copay): A fixed dollar amount you must pay with your own money for medical services, like office visits or prescription drugs.
Deductible: The amount you pay each year before your health plan begins paying.
Coinsurance: The percentage of costs for care that you'll pay - usually after you've paid your deductible.
Why did my costs change this year?Your health care costs can change for a number of reasons. The cost of care rising, the amount of people sharing the costs changing or a manufacturer raising or lowering their price on a drug are a few examples. If you’d like to discuss a specific change, click here to contact us, and we’ll try to answer your questions.
How do I pay my premium or change my payment information?This depends on your plan. For most plans, you can do a bank draft, check by phone, or mail in payment. Contact us and we’ll talk you through it or you can download the form here.
 How do I get one of my drugs covered?
How do I get one of my drugs covered? First, talk with your doctor about any generic versions or other drugs on your drug list that might work just as well. If we don’t cover a drug you need, your doctor can send us a request to cover it if they feel it’s important to your treatment. We’ll consider the request and get back to you on our decision.
How do I find a pharmacy in my network?You can search for pharmacies by network in the Find Care tool. Either search by the pharmacy’s name or search for ones near you and filter your results by your network. If you log in to bcbst.com first, your search results will automatically list pharmacies in your network. Need more help? Click here to contact us.
What do the drug 'tiers' mean?When a new drug becomes available, they’re put into one of three categories, or “tiers.”
Tier One: Generic drugs. These drugs are made with the same active ingredients and in the same dosage as the brand-name product, but cost less. They meet the same FDA standards as brand drugs and work just as well.
Tier Two: Preferred brand name drugs. These are the most affordable brand-name drugs.
Tier Three: Non-Preferred drugs. These are more expensive brand-name drugs. Often there are other similar ones available at a lower cost in one of the other two categories.
What are “preferred” drugs or pharmacies?Our doctors and pharmacists create a list of preferred drugs to put in our formulary (your list of covered drugs). Our drug list includes preferred generic (Tier 1) and preferred brand name (Tier 2) drugs. Non-preferred brand name (Tier 3) drugs are not part of the preferred drug list, but are covered by your pharmacy benefits, just at a higher cost.
Some plans have a list of “Preferred Pharmacies” that have agreed to keep costs even lower for our members and you’ll save money if you use them instead of a standard one in your network.
What is a specialty pharmacy or drug?A specialty drug is a prescription drug that is given by injection or infusion, sometimes by you and sometimes in the doctor’s office. You’ll often get the best price for your medicine by getting it from certain specialty pharmacies, even if it’s your doctor or preferred facility doing the procedure. Learn more.
In this issue...
- POLICY AND BILLING GUIDANCE
- PHARMACY UPDATES
- ALL PROVIDERS
Policy and Billing Guidance
Statewide Patient Centered Medical Home Incentives: Revised Policy and Billing Requirements
Effective July 1, 2013, New York State Medicaid is changing the reimbursement policy and billing requirements for providers recognized as Patient Centered Medical Homes (PCMH) by the National Committee for Quality Assurance (NCQA). The new policy applies to both Medicaid managed care and fee-for-service (FFS) and is consistent with the Medicaid Redesign Team’s (MRT) Triple Aim to improve care, improve health and reduce per capita costs.
The revised PCMH policy gives providers a fiscal incentive to achieve NCQA PCMH recognition using the 2011 versus the 2008 PCMH standards. The 2011 standards 'raise the bar' in terms of integrating behavior health and physical health care management and rewards clinicians for using health information technology to improve quality of care. The newer standards also promote robust patient centeredness goals to drive overall quality improvement.
The table below summarizes the Medicaid managed care PMPM and FFS 'add-on' amounts by provider type and recognition status as of July 1, 2013. Incentive payments for Level 2 NCQA PCMH recognized providers achieved using the 2008 NCQA standards will be eliminated. Level 2 incentive payments will remain at $4PMPM and $11.25 and $14.25 per visit in FFS, if recognized under the NCQA 2011 PCMH standards.
Level 3 PCMH providers, who achieved their recognition under the NCQA 2008 standards, will have their incentive payments reduced to $5PMPM and $14.05 and $17.85 per visit for FFS. Medicaid managed care reductions will be effective as of July 1, 2013. FFS reductions will be retroactive to July 1, 2013, contingent upon completion of eMedNY system edits. When a provider achieves PCMH recognition using the NCQA 2011 standards, their PCMH incentive payments will be reinstated at a higher level (see table below).
PROFESSIONS:
Medicaid coverage may be available for care and services that were necessary for the treatment of an 'emergency medical condition'. Per federal regulation the term emergency medical condition is defined as a medical condition (including emergency labor and delivery) manifesting itself by acute symptoms of sufficient severity (including severe pain) such that the absence of immediate medical attention could reasonably be expected to result in:
- (a) placing the patient's health in serious jeopardy;
- (b) serious impairment to bodily functions; or
- (c) serious dysfunction of any bodily organ or part.'
Patients whose drug coverage is limited may receive a pharmacy reason response of 'Patient is Not Covered', for drugs that do not meet the definition of 'emergency medical condition'. Providers can then verify if a patient has coverage for 'emergency services only', based on the reason response, by performing an eligibility request on ePACES; found under the eMedNY Tools Center at: https://www.emedny.org/index.aspx The Eligibility Response for these patients will return, 'emergency services only'.
Provided below is a link to the Department of Health’s MRT webpage where you can access background information and communication about this initiative and a list of emergency services covered drugs (scroll to the bottom of the page). http://www.health.ny.gov/health_care/medicaid/redesign/supplemental_info_mrt_proposals.htm
Please note:
- Short acting narcotics should only be written for an emergency five day supply.
- HIV prophylaxis therapy following occupational exposure & non occupational exposure (sexual assault) can be obtained via an exception process by following the procedure below.
Override Requests: Exception/override requests require a letter of medical necessity, providing rationale as to why this request meets the federal definition of an emergency medical condition as described above for the following medication(s). Please title request 'emergency services only,' and send to the ppno@health.state.ny.us mailbox or fax in to 518-473-5508 for review by a Medical Director. For questions on this policy providers may e-mail the pharmacy mailbox at: ppno@health.state.ny.us, or call (518) 486-3209. For questions on performing eligibility request on ePACES, providers may contact Computer Sciences Corporation at (800) 343-9000.
New York City Fee-for-Service Transportation Management Now Includes the Offices of Mental Health and Persons with Developmental Disabilities
Currently, the transportation of enrollees who reside in New York City and whose Medicaid eligibility is with the New York State Office of Mental Health (OMH, county code 97) or Office for People with Developmental Disabilities (OPWDD, county code 98) has been handled in one of two ways:
- 1. When the cost of transportation is included in the rate paid to a Medicaid program, that program arranges transportation to and from that program; or,
- 2. When transportation is fee-for-service, prior authorization of transportation is generated by the OMH or OPWDD central office staff located in Albany.
Effective June 1, 2013, the arrangement of fee-for-service transportation of these enrollees residing in New York City will be undertaken by the Department of Health's contracted transportation manager, LogistiCare Solutions (LGTC).
For dates of service on or after June 1, 2013, the ordering medical provider must seek authorization from LGTC instead of OMH or OPWDD central office staff. Staff in each agency's Albany-based central office will not process prior authorization requests with service dates on or after June 1, 2013. To secure approval prior to the trip, please call LGTC at (877) 564-5925. Trips performed without prior approval from LGTC will not be honored.
Ambulance vendors providing emergency transport to these enrollees must seek authorization from LGTC for the correct reimbursement within 90 days of the date of service.
Information regarding Medicaid transportation in NYC, including required forms and a list of participating transportation vendors, is available online at:
The LGTC Outreach Manager is available to visit each medical facility to discuss the process for requesting transportation authorization through LGTC. To request a visit, please call LGTC at (877) 564-5911.
Care at Home (CAH) III, IV and VI Case Management Providers: Delayed Implementation of the OPWDD Care at Home Waiver
Previously published in the December 2012 Medicaid Update, the Office for People with Developmental Disabilities (OPWDD) and the New York State Department of Health (DOH) are working with the Centers for Medicare & Medicaid Services (CMS) to combine CAH III, IV and VI into a single 1915(c) waiver program. The new waiver will be known as the OPWDD Care At Home Waiver. The purpose of this consolidation is to streamline and strengthen New York State's administrative oversight and reporting mechanism for these waiver programs.
Although it was anticipated that the new waiver would be implemented as of April 1, 2013, this update is to inform providers that implementation will be delayed until further notice due to outstanding review and approval by CMS. Providers will receive further notification and guidance when this consolidated waiver is approved and ready for implementation.
If you have questions about the new OPWDD Care At Home Waiver, please contact Lynda Baum-Jakubiak at (518) 474-5647 or the Division of Program Development and Management at (518) 473-2160.
New York Medicaid Electronic Health Records Incentive Program Update
The New York Medicaid EHR Incentive Program provides financial incentives to eligible practitioners and hospitals to promote the transition to electronic health records (EHR). Providers who practice using EHRs are in the forefront of improving quality, reducing costs, and addressing health disparities. Since December 2011 over $355.1 million in incentive funds have been distributed to over 5,925 New York State Medicaid providers.
For more information about the EHR Incentive program, we encourage you to visit the program website at https://www.emedny.org/meipass/ or attend one of the informational webinars hosted by the New York State Department of Health. To see the complete schedule of events and webinars, please view our Upcoming Events Calendar at: https://www.emedny.org/meipass/info/Events.aspx.
ATaking a Closer Look: Incentive Payments Paid to Healthcare Practitioners*(PDF, 510KB, 1pg.)
Medicaid Expanded Coverage for Diabetes Self-Management Training (DSMT)
Medicaid began reimbursing for Diabetes Self-Management Training (DSMT) effective January 1, 2011, when provided by an Article 28 clinic (hospital outpatient department or free-standing diagnostic and treatment center) accredited by a CMS approved national accreditation organization (NAO). Currently, CMS recognizes the American Diabetes Association (ADA), American Association of Diabetes Educators (AADE) and Indian Health Services (IHS) as approved NAOs. Under this accreditation, DSMT may be performed by a New York State licensed, registered, or certified professional in one of the following professional disciplines:
- Registered Nurse
- Registered Nurse Practitioner
- Registered Dietician
- Physician (MD, DO)
- Pharmacist
- Physician Assistant
- Physical Therapist
DSMT services may be provided to beneficiaries who are newly diagnosed with diabetes, to beneficiaries with diabetes who are stable, or to enrollees with diabetes who have a medically complex condition such as poor control of diabetes or other complicating factor. Adults with diabetes, who reported taking a course or class on how to manage their diabetes, were more likely to monitor their blood glucose daily (NYSBRFSS - Behavioral Risk Factor Surveillance System).
Diabetes Self-Management Education (DSME) is an essential element of diabetes care, and recently updated National Standards for Diabetes Self-Management Education and Support are based on evidence for its benefits. In New York State, there are 150 ADA/AADE recognized DSME programs. Education helps people with diabetes initiate effective self-management and cope with diabetes when they are first diagnosed. Ongoing DSME also helps people with diabetes maintain effective self-management throughout a lifetime of diabetes as they face new challenges and treatment advances become available. DSME helps patients optimize metabolic control, prevent and manage complications, and maximize quality of life in a cost-effective manner (2013 ADA Clinical Practice Recommendations).
DSMT services can be provided in individual sessions, or in group sessions of no more than eight patients. Claims must include the appropriate ICD-9 code for diabetes mellitus: 250.XX, 648.0x, 648.8x, 775.0, or 775.1. DSMT services are billed in unit increments with one unit equaling 30 minutes of service using the following HCPCS codes:
- G0108 - Diabetes outpatient self-management training services, individual, per 30 minutes.
- G0109 - Diabetes outpatient self-management training services, group (2-8 patients), per 30 minutes.
No more than 10 hours, or 20 units of diabetes self-management training for a newly diagnosed beneficiary or beneficiary with a medically complex condition can be billed during a continuous six-month period. Beneficiaries who are medically stable can receive up to 1 hour, or 2 units, of diabetes self-management training in a continuous six-month period.
In order to bill for DSMT services, Article 28 clinics will need to request an enrollment form by contacting Medicaid's Rate Based Provider Enrollment Office at (518) 474-8161. To avoid reimbursement interruption providers are advised to notify Rate Based Provider Enrollment upon re-certification from the NAO. Medicaid will also continue to reimburse for DSMT services provided by Certified Diabetes Educators (CDEs).
FOR ADDITIONAL INFORMATION PLEASE CONTACT:
- Billing and claims submission: eMedNY Call Center at (800) 343-9000.
- DSMT enrollment forms: Division of Provider Relations and Utilization Management at (518) 474-8161.
- DSMT coverage: Division of Financial Planning and Policy at (518) 473-2160.
Be Aware. Don't Share: State Health Commissioner Offers Tips on Insulin Pen Safety
Healthcare providers and diabetic patients in New York State may be tempted to reuse insulin pens on multiple patients to save money or stretch sometimes-scarce resources, but the New York State Department of Health (DOH) warns that this is a dangerous practice and should be discontinued immediately, as it poses a health risk to patients, even if the needle is changed between patients.
'Insulin pens, which are used to inject insulin into the body for the treatment of diabetes, contain more than one dose of insulin, are only meant for one person and should never be re-used from patient to patient.' State Health Commissioner, Nirav R. Shah, M.D., M.P.H., said. 'Back flow of blood into the insulin reservoir can occur during an injection. This creates a risk of bloodborne and bacterial pathogen transmission if the pen is used for more than one person, even when the needle is changed.'
DOH has been at the forefront of the national effort to eliminate unsafe injections, becoming one of the first two 'partner states' in the Safe Injection Practices Coalition's (SIPC) One & Only Campaign in 2009. The SIPC is a partnership of healthcare-related organizations led by the Centers for Disease Control and Prevention (CDC) that was formed to promote safe injection practices in all U.S. healthcare settings. The New York One & Only Campaign's activities are supported by a CDC grant.
During 2009, in response to reports of improper use of insulin pens in hospitals, the Food and Drug Administration (FDA) issued an alert for healthcare professionals reminding them that insulin pens are meant for use on a single person and are not to be shared. Unfortunately, there have been continuing reports throughout the U.S., of persons placed at risk of disease from viruses like hepatitis B (HBV), hepatitis C (HCV) and HIV, through sharing of insulin pens or other injectable devices.
In 2011, DOH identified transmission of hepatitis B virus between two patients at a residential healthcare facility. Specifically, staff members were performing fingersticks using a shared lancet pen. The lancets were replaced after each test, but the pen was shared among multiple patients.
To prevent transmission of bloodborne or bacterial disease, these CDC recommendations should be followed by both patients and providers:
- Fingerstick devices (including lancet pens and lancets) should never be used for more than one person.
- Whenever possible, blood glucose meters should not be shared. If they must be shared, the device should be cleaned and disinfected after every use, per manufacturer's instructions. If the manufacturer does not specify how the device should be cleaned and disinfected then it should not be shared.
- Insulin pens and other medication cartridges and syringes are for single-patient-use only and should never be used for more than one person. After use, all sharp fingerstick equipment must be disposed of at the point of use in an approved sharps container.
Additional information on the 'Be Aware. Don't Share' program, is available at: http://www.oneandonlycampaign.org/content/insulin-pen-safety.
Medicaid to Implement Changes for Hospitals and Nursing Home Claims Processing
Effective June 21, 2013, Medicaid will implement new claims editing to ensure patient responsibility amounts are deducted from the appropriate inpatient hospital or nursing home claim, and that claims for nursing home services (excluding leave of absence stays) are not reimbursed when the Medicaid beneficiary is in an inpatient hospital setting.
Duplicate Claims
Edit 02224 - 'Inpatient/Nursing Home Duplicate' will deny inpatient hospital or nursing home claims with overlapping dates of service unless the nursing home claim contains one of the following revenue codes:
- 0183 - Therapeutic Leave
- 0185 - Hospital Leave
- 0189 - Therapeutic Leave Authorized by a Medical Professional
A nursing home resident should not be in a hospital inpatient setting unless the nursing home resident is on a leave of absence. Please refer to the Edit Error Knowledge Base (EEKB) to see the Claim Adjustment Reason Code eMedNY will provide for this Edit. EEKB information is posted on eMedNY.org at: https://www.emedny.org/HIPAA/edit_error/knowledgebase.aspx.
Note: The conflicting claim will be reported on the provider's remittance statement.
Claims Involving Patient Responsibility Amounts (NAMI and Inpatient Hospital Patient Liability)
Effective June 21, 2013, there will be changes to claim reductions for Net Available Monthly Income (NAMI) amounts and Inpatient Hospital Patient Liability amounts as follows:
Net Available Monthly Income (NAMI)
NAMI reductions will be assessed to the entity in which the client 'resides' on the first day of the month:
- When an inpatient claim is received for a client responsible for NAMI, the NAMI amount will be deducted from the hospital inpatient claim.
- When a nursing home claim is received that includes the first day of the month, the nursing home will be assessed the reduction.
The one exception to this rule is the hospital will not be assessed the NAMI when a nursing home claim for a bed reservation spans the same first day of the month.
When a paid hospital inpatient claim:
- includes the first day of the month;
- is reduced by the NAMI, and
- a subsequent nursing home claim indicating leave of absence is processed, the nursing home claim will have the NAMI deducted and eMedNY will automatically process an adjustment to the hospital inpatient claim to reverse the NAMI deduction.
Inpatient Hospital Patient Liability
- If an entry of an Inpatient Hospital Patient Liability amount is delayed by the responsible local agency enabling the applicable Inpatient Hospital claim to be paid prior to the eMedNY system being aware of the liability, eMedNY will automatically recognize and adjust the paid claim(s) to deduct the Patient Liability amount(s).
NAMI and Inpatient Hospital Patient Liability Amounts
- For Medicaid beneficiaries who have an Inpatient Hospital Patient Liability on file, the amount will be returned in the Eligibility Response along with the corresponding Begin and End Dates.
- For Medicaid Beneficiaries who have a NAMI Amount on file, the amount will be returned in the Eligibility Response along with the NAMI Begin Date.
Questions should be directed to mailto eMedNYHIPAASupport@csc.com.
Medicaid to Implement Changes to Eligibility Inquiry/Response Transactions (ASC X12 270/271)
Effective July 2011, the Department of Health and Human Services (DHHS) published an Interim Final Rule to adopt the Operating Rules for Eligibility for a Health Plan transactions. eMedNY plans to implement system enhancements related to the federal mandate to the Eligibility Transaction Inquiry/Response on June 21, 2013. The eligibility transaction changes will also affect users of ePACES. Updated ePACES Quick Reference Guides that reflect the changes for both eligibility inquiry and response will be available on the eMedNY website.
Generic Service Type Request/Response
The HIPAA Version 5010 standard was implemented by Medicaid on July 21, 2011. Since then, eMedNY has treated all eligibility requests as generic. This means that even if an eligibility request is received for an explicit Service Type, eMedNY returns any or all of the following Service Type codes (EB03), if such coverage exists for the Medicaid beneficiary:
- 1 - Medical Care Code
- 33 - Chiropractic
- 35 - Dental Care
- 47 - Hospital
- 48 - Hospital Inpatient
- 50 - Hospital Outpatient
- 86 - Emergency Services
- 88 - Pharmacy
- 98 - Professional (Physician) Visit - Office
- AL - Vision (Optometry)
- MH - Mental Health
- UC - Urgent Care
Explicit Service Type Request/Response
Effective June 21, 2013, submitters of 270 transactions will be able to submit Service Type explicit requests while continuing to be able to submit the current generic eligibility requests (EQ01 [Service Type] = 30). The Service Type explicit requests include the types listed in the table above plus the additional ones listed in the second table below. If a Service Type code other than one from these tables is submitted, eMedNY will respond with a generic response. Please see the notes below the second table.
- 2 - Surgical
- 4 - Diagnostic X-ray
- 5 - Diagnostic Lab
- 6 - Radiation Therapy
- 7 - Anesthesia
- 8 - Surgical Assistance
- 12 - Durable Medical Equipment Purchase
- 13 - Ambulatory Service Center Facility
- 18 - Durable Medical Equipment Rental
- 20 - Second Surgical Opinion
- 40 - Oral Surgery
- 42 - Home Health Care
- 45 - Hospice
- 51 - Hospital Emergency Accident
- 52 - Hospital - Emergency Medical
- 53 - Hospital - Ambulatory Surgical
- 62 - MRI/CAT Scan
- 65 - Newborn Care
- 68 - Well Baby Care
- 73 - Diagnostic Medical
- 76 - Dialysis
- 78 - Chemotherapy
- 80 - Immunizations
- 81 - Routine Physical
- 82 - Family Planning
- 93 - Podiatry
- 99 - Professional (Physician) Visit Inpatient
- A0 - Professional (Physician) Visit Outpatient
- A3 - Professional (Physician) Visit Home
- A6 - Psychotherapy
- A7 - Psychiatric Inpatient
- A8 - Psychiatric Outpatient
- AD - Occupational Therapy
- AE - Physical Medicine
- AF - Speech Therapy
- AG - Skilled Nursing Service
- AI - Substance Abuse
- BG - Cardiac Rehabilitation
- BH - Pediatric
Providers using the Audio Response Unit (ARU) (telephone) and the Point of Service (POS) device will receive a new prompt to enter Service Type explicit requests.
Notes:
ARU-only one Service Type explicit code may be entered per transaction. POS device-up to 10 Service Type explicit codes may be entered per transaction.
Other Coverage Responses Beginning on June 21, 2013, when the Medicaid beneficiary is enrolled in a Medicaid Managed Care plan or Family Health Plus, carve-outs for Pharmacy, Family Planning or Mental Health will be returned if applicable. A literal returned in EB05 = 'ELIGIBLE PCP' or 'FAMILY HEALTH PLUS' will indicate coverage within a plan. The first iteration of the EB segment will be returned as follows:
EB01 = U [Contact Following Entity for Eligibility or Benefit Information]
Uc Copay Meaning
Multiple iterations of the EB segment may be returned to indicate carve-outs, if applicable:
- EB01 = 1 [Active Coverage],
- EB03 = 88 [Pharmacy]
- EB01 = 1 [Active Coverage],
- EB03 = 82 [Family Planning]
- EB01 = 1 [Active Coverage],
- EB03 = MH [Mental Health]
The ARU method will return the following literals when such coverage exists:
- Eligible PCP With Family Planning Carve Out (Only)
- Eligible PCP With Family Planning and Pharmacy Carve Out
- Eligible PCP With Mental Health and Family Planning Carve Out
- Family Health Plus with Family Planning Carve Out (Only)
- Eligible PCP With Mental Health and Family Planning and Pharmacy Carve Out
- Family Health Plus with Family Planning and Pharmacy Carve Out
Medicaid Copay Changes
Today, eligibility responses contain information about the yearly copay for the patient's annual remaining amount (EB01 = B). Beginning on June 21, 2013, eMedNY will respond with Medicaid's standard copay amounts for the service type requested when there is an annual copay amount remaining.
For generic requests, eMedNY will return the standard copay amount for each explicit Service Type for which there is a covered response when there is an annual copay amount remaining. When EB01 = B for copay, the EB03 = service type category and its corresponding EB07 = standard copay amount is as follows:
| Code | Description |
| 231 | Eligible Only Outpatient Care |
| 232 | Outpatient Coverage with Community-Based Long Term Care |
| 233 | Outpatient Coverage without Long Term Care |
| 234 | Outpatient Coverage with No Nursing Facility Services |
| 235 | Eligible PCP with Family Planning Carve Out (Only) |
| 236 | Eligible PCP with Mental Health and Family Planning Carve Out |
| 237 | Eligible PCP with Mental Health, Family Planning and Pharmacy Carve Out |
| 238 | Eligible PCP with Family Planning and Pharmacy Carve-Out |
| 239 | Family Health Plus with Family Planning Carve-Out (Only) |
| 240 | Family Health Plus with Family Planning and Pharmacy Carve-Out |
Future Date Eligibility Requests
Current eMedNY functionality allows eligibility verifications for today’s date and any date in the past up to two years prior. Beginning June 21, 2013, eligibility may be performed for any date within the current month even if it is a future date. Eligibility requests for dates in subsequent months will not be allowed. For example on July 1, 2013, a request may be submitted for any date during the month of July but not beyond July 31. Providers should still verify eligibility on date of service.
More details will be available in the MEVS/DVS Manual (when available) located at:
Please be sure you are signed up for the eMedNY Listserv® to be notified when updates are available to a Provider Manual like the MEVS/DVS manual. To sign-up for the listserv 'eMedNY General Updates' list, visit www.emedny.org.
In addition, prior to the June implementation, more information will be made available in the transaction Information Companion Guide, available on the eMedNY website at:
Questions can be directed to eMedNYHIPAASupport@csc.com.
The New York State Medicaid Prescriber Education Program Drug Information Response Center Addresses Dry Cough Associated with Linagliptin
The New York State Medicaid Prescriber Education Program (NYSMPEP) is a collaboration between the New York State Department of Health (NYSDOH) and the State University of New York (SUNY), as approved by state legislation. This program was designed to provide prescribers with an evidence-based, non-commercial source of the latest objective information about pharmaceuticals. In conjunction, the Drug Information Response Center (DIRC) was developed to fulfill the mission of assisting clinicians in the delivery of health care to their Medicaid patients by providing timely, evidence-based information on pharmacotherapy to prescribers and serving as a resource for NYSMPEP academic educators in their outreach to prescribers. A recent article was prepared by the DIRC regarding the association between linagliptin and dry cough.
Linagliptin (Tradjenta®) is a dipeptidyl peptidase-4 (DPP-4) inhibitor that is approved to treat type 2 diabetes mellitus (T2DM) in adults.¹ Though generally well tolerated, some adverse effects have been reported to occur more commonly in patients taking linagliptin, including cough. According to the linagliptin prescribing information, cough was reported to occur in 2.1% of linagliptin-treated patients (n=3,625) compared to 1.4% of patients treated with placebo (n=2,176) for either linagliptin monotherapy or combination therapy over a mean period of 29.6 weeks. The medical review of all data submitted by the manufacturer to the Food and Drug Administration (FDA) Center for Drug Evaluation and Research prior to approval of linagliptin revealed a higher incidence of cough with linagliptin compared to all other regimens.² These regimens included placebo, metformin, a sulfonylurea, metformin and a sulfonylurea, or a thiazolidinedione. The incidence of cough in linagliptin treated patients ranged from 0.4% to 2.4% while the incidence in patients on comparators ranged from 0% to 1.2%.
From a search of the literature, studies were identified in which cough was reported in patients receiving linagliptin. Schernthaner et al. conducted a pooled analysis of 8 double-blind, randomized, phase III studies of <24 weeks duration that compared linagliptin to placebo.³ A total of 2,523 patients received linagliptin 5 mg daily and 1,049 patients received placebo. The mean age was approximately 57 years; 51.1% of patients receiving linagliptin were male, and approximately half had a history of diabetes >5 years. Cough was reported in 1.7% of patients receiving linagliptin versus 1.0% of patients receiving placebo (p-value not reported). The overall incidence of adverse events was similar between groups (55.8% for linagliptin versus 55.0% for placebo).
More recently, Gallwitz et al. conducted a 2-year trial comparing the safety and efficacy of linagliptin to that of glimepiride in patients with T2DM inadequately controlled on metformin.(4)
REFERENCE:
- 1) Linagliptin (Tradjenta) prescribing information. Boehringer Ingelheim Pharmaceuticals, Inc. Ridgefield, CT 2012. http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/201280s005lbl.pdf. Accessed January 24, 2013.
- 2) Dunn S. Linagliptin Medical Review. Center for Drug Evaluation and Research. 2011; http://www.accessdata.fda.gov/drugsatfda_docs/nda/2011/201280Orig1s000MedR.pdf. Accessed January 24, 2013.
- 3) Schernthaner G, Barnett AH, Emser A, et al. Safety and tolerability of linagliptin: a pooled analysis of data from randomized controlled trials in 3572 patients with type 2 diabetes mellitus. Diabetes, obesity & metabolism. May 2012;14(5):470-478.
- 4) Gallwitz B, Rosenstock J, Rauch T, et al. 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet. Aug 4 2012;380(9840):475-483.
- 5) Saxagliptin (Onglyza) prescribing information. Bristol-Myers Squibb Company. Princeton, NJ. 2011; http://www.accessdata.fda.gov/drugsatfda_docs/label/2011/022350s004lbl.pdf. Accessed January 24, 2013.
- 6) Sitagliptin (Januvia) prescribing information. Merck & Co, Inc. Whitehouse Station, NJ. 2012; http://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021995s025lbl.pdf. Accessed January 24, 2013.
Patients with a glycosylated hemoglobin of 6.5% to 10% already on metformin or metformin plus 1 additional antidiabetic agent (which was discontinued during a washout period) were given linagliptin 5 mg daily (n=777) or glimepiride 1-4 mg daily (n=775). The mean age was approximately 60 years; approximately 60% of each group was male, and approximately 50% had a history of T2DM >5 years. Over the study period, cough occurred in 6.1% of patients receiving linagliptin compared to 4.9% of patients receiving glimepiride (p-value not reported). Overall, fewer adverse events were reported in the linagliptin group compared to the glimepiride group.
Of note, in a brief review of the prescribing information for the other FDA approved DPP-4 inhibitors, sitagliptin (Januvia®) and saxagliptin (Onglyza®), cough was not observed.5,6 These data suggest that cough may not be a class-related adverse effect.
Based on the information provided by the manufacturer and clinical trials, linagliptin does appear to be associated with cough, at a higher incidence compared to placebo and other antidiabetic agents. The incidence of cough may be duration-dependent, as a higher incidence was reported in the longer trial. It is unclear if this adverse effect resolves upon discontinuation of the linagliptin. If a patient is unable to tolerate linagliptin, substitution with another DPP-4 inhibitor may be considered.
To contact an NYSMPEP academic educator in your area, please visit http://nypep.nysdoh.suny.edu/contactus/contactus.
Guidance for Pharmacies on New Prospective Drug Utilization Review (DUR) Edit
The Medicaid fee-for-service (FFS) program will be implementing a new prospective DUR edit (02120) 'Prescriber Notification' to comply with recommendations of the DUR Board. This edit is designed to aid pharmacists when optimal therapy may not be reflected in the recipient’s claim history. Pharmacists will have the right to exercise professional judgment with the ability to override the edit, when an informed decision on therapy has been reached.
System messaging has been developed to help guide the pharmacists to appropriately submit the claim or consult with the prescriber. In the future, there will be clinical criteria applied to therapeutic classes and individual medications. As clinical criteria are developed, the Department will inform providers prior to activating the edits to reject claims.
For claims that do not meet clinical criteria, eMedNY POS will return a rejected response similar to the prospective DUR edits in place today (i.e. Therapeutic Duplication (TD) and Drug-Drug Interaction (DD)).
- Reject response (NCPDP field 511-FB) '88 - DUR Reject ERROR'
- Conflict code (NCPDP field 439-E4) 'PN (Prescriber Notification)'
- Additional detailed messages (NCPDP field 544-FY): This is a free form field to identify the potential issue.
If a claim transaction is rejected due to this DUR edit and you intend to dispense the drug, you will need to override the reject (if appropriate). In order to process the override, the matching conflict code that was returned as the denial code must be placed in the Reason for Service Code (439-E4) field, ('PN' must be placed in the Reason for Service Code field). The DUR Conflict Code being sent as the override must match the Conflict Code received in the response of the original transaction. A corresponding entry must also be entered in the Result of Service Code (441-E6) field and appropriate Submission Clarification Code (420-DK).
Result of Service Code (441-E6) Examples
- 1A = Filled as is, false positive
- 1B = Filled, Prescription As Is
- 1G = Filled with Prescriber Approval
Submission Clarification Codes (420-DK)
- 05 = Therapy Change
- 06 = Starter Dose
- 07 = Medically Necessary
A full list of Result of Service codes can be found in the ProDUR-ECCA D.0 Provider Manual at:
eMedNY 5010/D.0 transaction instructions are available online at:
For questions on either of these transactions, providers may contact the eMedNY Call Center at (800) 343-9000.
Caution Urged When Nursing Facilities Use Antipsychotics
On March 6, 2013, the Commissioner of Health and the Office of the Medicaid Inspector General (OMIG) jointly issued a letter to all nursing facilities urging caution about the unnecessary use of antipsychotic drugs. Antipsychotics have significant and profound risks including death when used in nursing facilities, and there is concern that antipsychotics, at times, are being used unlawfully as a chemical restraint. In its review, the Inspector Genera'’s 2012 report found that, almost all resident assessments and/or care plans for nursing home residents using antipsychotics were inadequate.
Nursing facilities are expected to have their entire interdisciplinary team, including the medical director, develop and review policies and procedures regarding the use of antipsychotic medication. The letter included a number of attachments to further educate nursing facilities about the use of antipsychotic medication, about the establishment of protocols and procedures, and about managing dementia and Alzheimer's disease.
The letter and its attachments are available online at: http://www.omig.ny.gov/images/stories/provider_misc/antipsychotics-4-9-13.pdf.
ALL PROVIDER
New Training Schedule and Registration
- Do you have billing questions?
- Are you new to Medicaid billing?
- Would you like to learn more about ePACES?
If you answered YES to any of these questions, you should consider registering for a Medicaid training session. Computer Sciences Corporation (CSC) offers various types of educational opportunities to providers and their staff. Training sessions are available at no cost to providers and include information for claim submission, Medicaid Eligibility Verification, Electronic Funds Transfer, Electronic/PDF Remittance Advice Form Completion and the eMedNY website.
Web Training Now Available
You can also register for a webinar in which training would be conducted online and you can join the meeting from your computer and telephone. After registration is completed, just log in at the announced time. No travel involved.
Many of the sessions planned for the upcoming months offer detailed instruction about Medicaid’s free web-based program ePACES which is the electronic Provider Assisted Claim Entry System that allows enrolled providers to submit the following type of transactions:
- Claims (Dental, Professional, Institutional
- Eligibility Verifications
- Claim Status Requests
- Prior Approval/DVS Requests
Uc Copay Meaning Definition
Physician, Nurse Practitioner, DME and Private Duty Nursing claims may even be submitted in 'REAL-TIME' via ePACES. Real-time means that the claim is processed within seconds and professional providers can get the status of a real-time claim, including the paid amount without waiting for the remittance advice.
Fast and easy registration, locations, and dates are available on the eMedNY Website at: http://www.emedny.org/training/index.aspx
CSC Regional Representatives look forward to having you join them at upcoming meetings!
Ucsd Pay Scale
If you are unable to access the Internet to register or have questions about registration, please contact the eMedNY Call Center at (800) 343-9000.
Provider Directory
Uc Copay Meaning Dictionary
- Office of the Medicaid Inspector General:
For suspected fraud complaints/allegations, call 1-877-87FRAUD, (877) 873-7283, or visit www.omig.ny.gov. - Provider Manuals/Companion Guides, Enrollment Information/Forms/Training Schedules: Please visit the eMedNY website at: www.emedny.org.
- Providers wishing to hear the current week's check/EFT amounts: Please call (866) 307-5549 (available Thursday PM for one week for the current week's amount)
- Do you have questions about billing and performing MEVS transactions? Please call the eMedNY Call Center at (800) 343-9000.
- Provider Training: To sign up for a provider seminar in your area, please enroll online at: http://www.emedny.org/training/index.aspx. For individual training requests, call (800) 343-9000 or e-mail: emednyproviderrelations@csc.com.
- Enrollee Eligibility: Call the Touchtone Telephone Verification System at (800) 997-1111.
- Need to change your address? Does your enrollment file need to be updated because you've experienced a change in ownership? Do you want to enroll another NPI? Did you receive a letter advising you to revalidate your enrollment? Visit www.emedny.org/info/ProviderEnrollment/index.aspx and choose the link appropriate for you (e.g., Physician, Nursing Home, Dental Group, etc.)
- Medicaid Electronic Health Record Incentive Program questions? Contact the New York Medicaid EHR Call Center at (877) 646-5410 for assistance.
- Do you have comments and/or suggestions regarding this publication?
- Please contact Kelli Kudlack at: medicaidupdate@health.state.ny.us.
